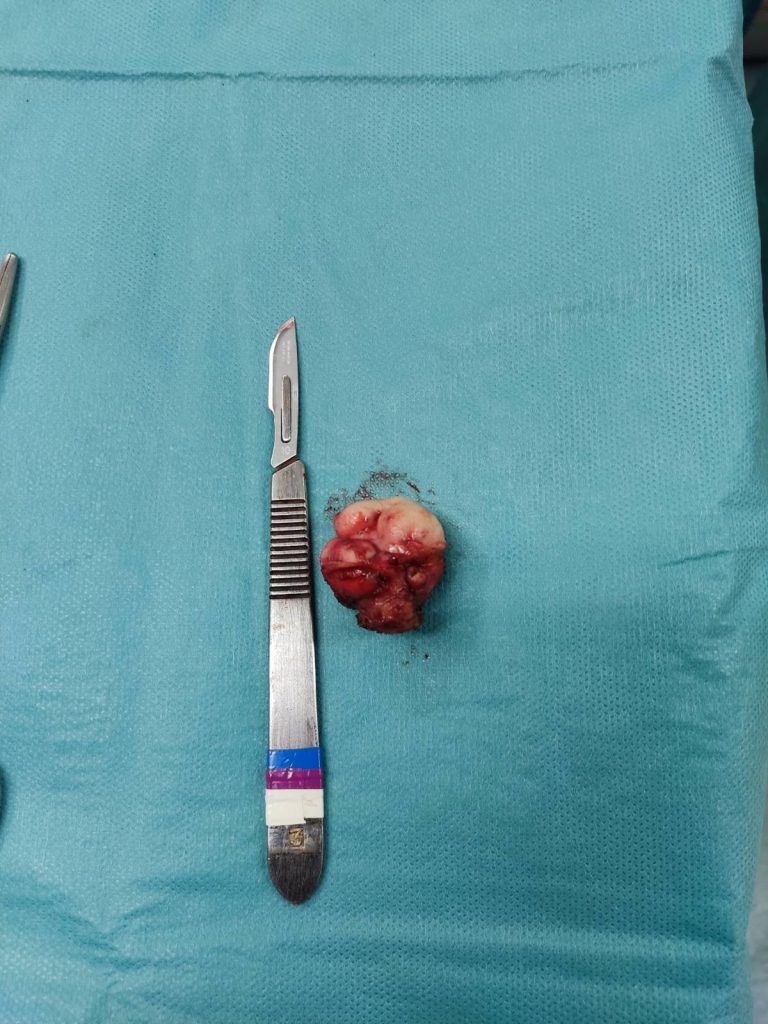
Umbilical endometriosis is defined as the presence of ectopic endometrial glands and stroma within the umbilicus. When the condition happens without prior surgery, it’s called primary umbilical endometriosis. This is a case report of a primary umbilical endometriosis operated in our centre. After excision of the nodule, the belly button was reconstructed.
Primary umbilical endometriosis
Primary umbilical endometriosis is considered a rare form of endometriosis, and according to some studies, one that is clinically difficult to differentiate from other diseases that cause umbilical nodules. However, in our patient case, as with most endometriosis sufferers, she diagnosed herself.
Case presentation
“Symptoms started 8 years ago, when I was 25. The only symptom for the first few years was mild pain in the umbilical area when I lay down on my stomach. I was misdiagnosed with umbilical hernia, but since I haven’t had a pregnancy yet, I was told to wait and have surgery after I give birth.
A few years later I started to have umbilical bleeding. The first time it happened surgeons in the ER said it wasn’t hernia but accused me of having poor hygiene that caused umbilical infection!
I realised it was endometriosis when umbilical bleeding started to repeat every month, right when I was on period”
Self-diagnosis with umbilical endometriosis

After years of noticing that with each period, she is bleeding from her umbilicus, our patient told doctors that she believes it is endometriosis. Although they have accepted and agreed that it is endometriosis, they have not offered her any treatment plan. Moreover, she was tossed from doctor to doctor.
“Gynaecologists would say that the umbilicus is not their area and they would refer me to general surgeons. General surgeons would say that it’s not their area either, because it was superficial, and would refer me to plastic surgeons. Plastic surgeons would say they know nothing about endo and refer me back to gynaecologist. This circle repeated every time I tried to get help. Sometimes someone asked for an ultrasound or MRI but then did nothing with these results”.
Extrapelvic endometriosis is usually accompanied by disease in other parts of the pelvis
Related to endometriosis in any other part of the body, there was suspicion but it was never confirmed. On multiple occasions I had blood in the sample when I did pap smear. I had two biopsies on my cervix, but they ruled out endo. Turned out that I also had endo protruding from my pelvis into the vaginal canal and probably this is where blood came from. I was always examined with a speculum so they didn’t catch it, they would have if they ever did a bimanual exam”.
Her proper diagnosis was with our centre
“Dinos was the first one to catch that one. He was also the first one to suggest doing MRI under endometriosis protocol. I had to do that in Athens too, as no radiologist heard about it in my country. I decided to travel to Greece after years of not receiving any treatment proposal in my country, and finding out about an excision specialist (which my country also didn’t have)”.
The impact of primary umbilical endometriosis
Whatever type of endometriosis one might have, the impact can be big. In our patient’s case, the primary umbilical endometriosis had a significant impact on her self-esteem, and at the same time, due to bleeding during periods, she needed to wear a pad.
“I was bleeding every month from my umbilicus, enough to bleed through the make up pad that I taped to my stomach, through my shirt and pants. It was painful and it was visibly growing. I had a tiny umbilicus but a big mass grew out in it and started sticking out which had a negative impact on my body image and self-confidence. I was also starting to consider pregnancy but was afraid what would happen with this mass in my belly button when I get pregnant and my stomach starts growing. It was discouraging me from even trying to.
After surgery she is doing well
“After the surgery I am doing well. Physical recovery was very quick, I was able to have long walks since day 4 after surgery. I have had two periods and have less menstrual cramps now. I used to take three painkillers per day for four days, now I take just one pill per day for the first two days. Also my periods are extremely regular now, they happen on the 28th day of the cycle which was never the case previously”.